Injections save vision
after
macular degeneration diagnosis

On December 30, 2006, Bee Epstein-Shepherd was returning from a trip, passing the time on the airplane by reading. When she got home, she turned on her computer, stared at a line of type that was supposed to be straight, and noticed that it looked wavy.
“I panicked, because I knew what it meant,” says Epstein-Shepherd, a doctor of clinical hypnotherapy who has built a career on helping people deal with fear and stress.
She was diagnosed with “wet” macular degeneration, a chronic eye disorder that her mother also had. It can cause blurred vision or a blind spot from abnormal blood vessels that leak fluid or blood. Most people diagnosed with age-related macular degeneration (AMD) have “dry” AMD, in which the central portion of the retina thins; vision is compromised, but there is no leakage or bleeding.
Seeing a straight line appear wavy was a strong indication that a vessel in Epstein-Shepherd’s eye was bleeding into her macula, the part of the retina responsible for central vision.
“In a matter of a few hours, from the time I got off the plane to the time I got home, my eye apparently had bled very quickly, so I immediately picked up the phone and called my ophthalmologist,” says the Carmel Valley resident.
“It was the Saturday night before New Year’s Eve, and Dr. (Eric) Del Piero responded right away,” Epstein-Shepherd says. “He saw the urgency and had me in his office at 8 o’clock Sunday morning, which showed exactly what kind of doctor he is.”
Wet macular degeneration is usually treated by injecting medications into the eye that can help stop the growth of new blood vessels. The injections may be needed as often as once a month. If vision has been lost or compromised due to the disease, it may be partially restored in some cases as the blood vessels shrink and the fluid is absorbed.
In Shepherd-Epstein’s case, regular treatments over the past 14 years have preserved her vision: At 83, she showed 20-25 vision in her right eye and 20-30 in her left in her most-recent exam.
The injections are done in the Outpatient Surgery Center at Community Hospital of the Monterey Peninsula.

Injections into the eye sound daunting, but Epstein-Shepherd, the professional stress reliever, offers this reassurance:
“They are painless, because your eye is numbed beforehand,” she says. “You’ll feel a little pressure, but, honestly, I feel a lot more pain if I get poked picking my roses than I’ve ever had from the injections.
“Doctors advise you to take Tylenol® if you experience any discomfort after a treatment, but I’ve never had to do that,” says Epstein-Shepherd, who estimates she’s had more than 50 injections since January 2007. “I can’t say I’ve ever had an unpleasant experience from the treatments I’ve received.”
Epstein-Shepherd also takes vitamins to boost eye health on her doctor’s advice, and says she’s experienced almost no loss of vision since she began the treatments.
“It’s been 14 years since we started,” she says, “and if my vision has changed at all, those changes have been so slow and so minimal that I hardly notice.”
"It’s been 14 years since we started, and if my vision has changed at all, those changes have been so slow and so minimal that I hardly notice."
— Bee Epstein-Shepherd, patient
Age-related macular degeneration
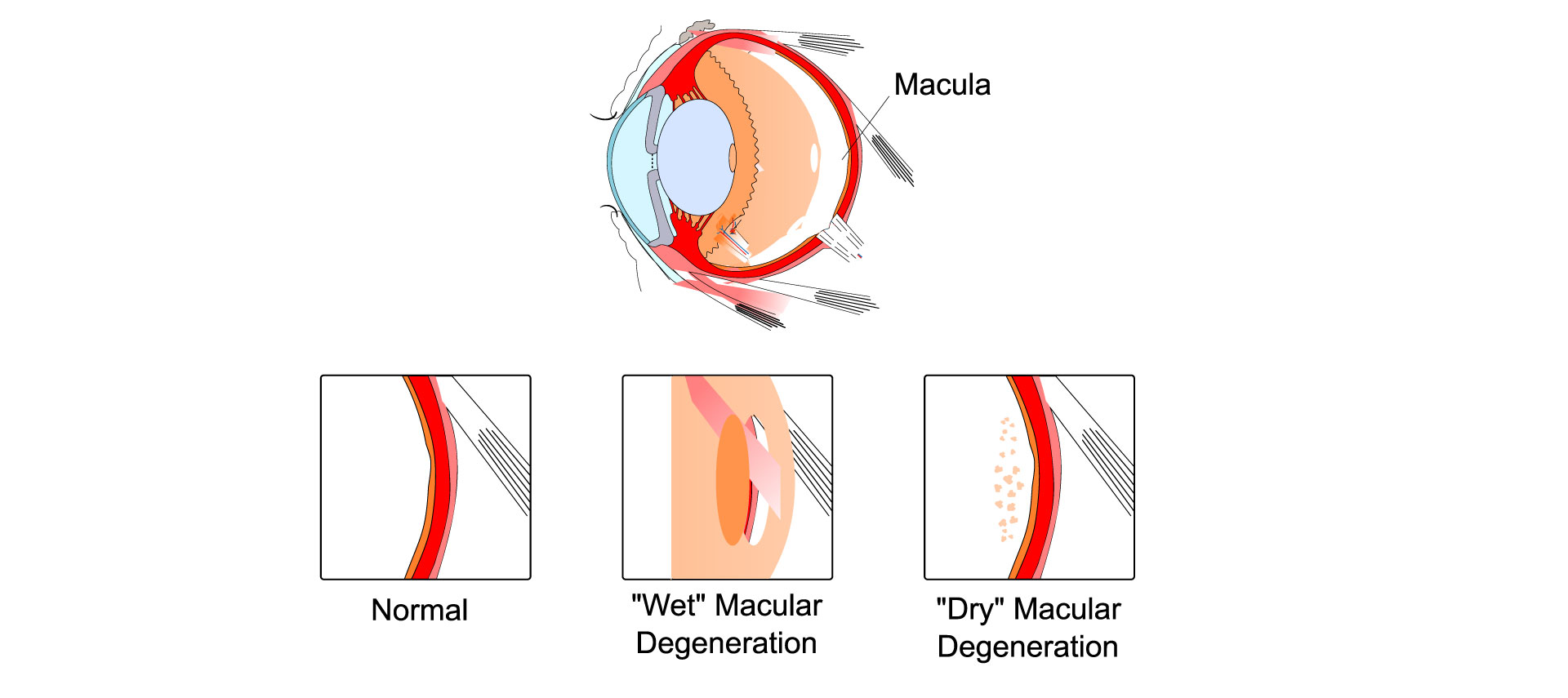
Age-related macular degeneration (AMD) affects the macula, or central area of the retina. It blurs central vision, making it hard to see faces, drive, or do close-up work. It is a leading cause of vision loss for people 50 and older.
Symptoms: Blurry area near center of vision; may get bigger or have blank spots over time.
In some cases, straight lines start to look wavy; if this happens, see an eye doctor right away
Risk factors: Age, family history of AMD,
white race, smoking
Prevention: Quit smoking, get regular physical activity, maintain healthy blood pressure and cholesterol, eat healthy foods, including leafy green vegetables and fish
Diagnosis: Dilated eye exam
Treatment: Vitamins and minerals, injections, laser treatment
SOURCE: National Institutes of Health
Eye interventions
More than 800 eye surgeries and procedures are performed annually at Community Hospital of the Monterey Peninsula, including:
- Surgery for:
- Retina detachment
- Diabetic retinopathy
- Holes or puckers in the macula, the central area of the retina
- Drooping eyelids and eyelid malposition
- Removing tumors
- Glaucoma surgery with valve insertion to reduce pressure
- Laser trabeculolasty to reduce eye pressure in patients with open-angle glaucoma
- Laser iridotomy to treat patients with narrow- or closed-angle glaucoma
- Transscleral selective laser treatments to reduce eye pressure in all forms of glaucoma
- Implants of sustained-release eye medications to treat glaucoma or other eye diseases
- Injections to treat macular degeneration and retinal circulatory problems
- Laser surgery to remove “secondary cataracts” or cloudy capsule membranes that can develop months or years after successful cataract surgery
- Lens implants during cataract surgery to correct astigmatism and both distance and near vision
- Intraocular gas/fluid exchange for persistent or recurring bleeding between the lens and retina
- Pneumatic retinopexy with cryotherapy for retinal detachments, in which a gas bubble is injected into the eye to push the retina against the back of the eye, and then is frozen in place
- Removal of foreign bodies
- Laceration repairs