Technology + human touch support
successful joint replacement

Steadily evolving medical technology has made joint replacement easier than ever before, but teamwork and a clear before-during-and-after plan among patient, surgeon, and hospital staff are critical to a successful outcome.
“It’s still a major operation, but what we’ve learned through the years is that patients do much better if they have a better understanding of the process, its risks and complications, and how important their own participation is in the outcome,” says Dr. Michael Pitta,
an orthopedic surgeon.
To help develop that understanding, the Orthopedic Center at Community Hospital of the Monterey Peninsula has added a dedicated nurse navigator to work with patients having knees, hips, or shoulders replaced, and an interactive software tool that helps guide them through the process. The software, from Force Therapeutics, has been used by Pitta, Dr. Christopher Meckel, and others at Monterey Spine & Joint for more than a year, generating positive response from patients.
“It has been a great way to stay connected, get the information I need, and feel well cared for,” says Meredith Manhard, who had a hip replacement by Dr. Christopher Meckel earlier this year. (See related story.)

"Force Therapeutics enables us to get information to our patients at the time they need it, and keep every member of our team on the same page with our plan."
— Dr. Christopher Meckel, Orthopedic surgeon
Through the Force software, medical teams can send information, reminders, and instructional videos to keep the patient on track before surgery and through recovery. It also allows patients, or their advocates, to communicate with those team members through secure texting, so they don’t have to navigate a phone system or track down the person who can address their issue.
Force is now also used by Dr. Scott Kantor and Dr. Gregg Satow and available to other Orthopedic Center surgeons.
“Force enables us to get information to our patients at the time they need it, and keep every member of our team on the same page with our plan,” says Meckel, “it wasn’t that we didn’t have a plan in previous years — it’s just that those plans weren’t always well-articulated.”
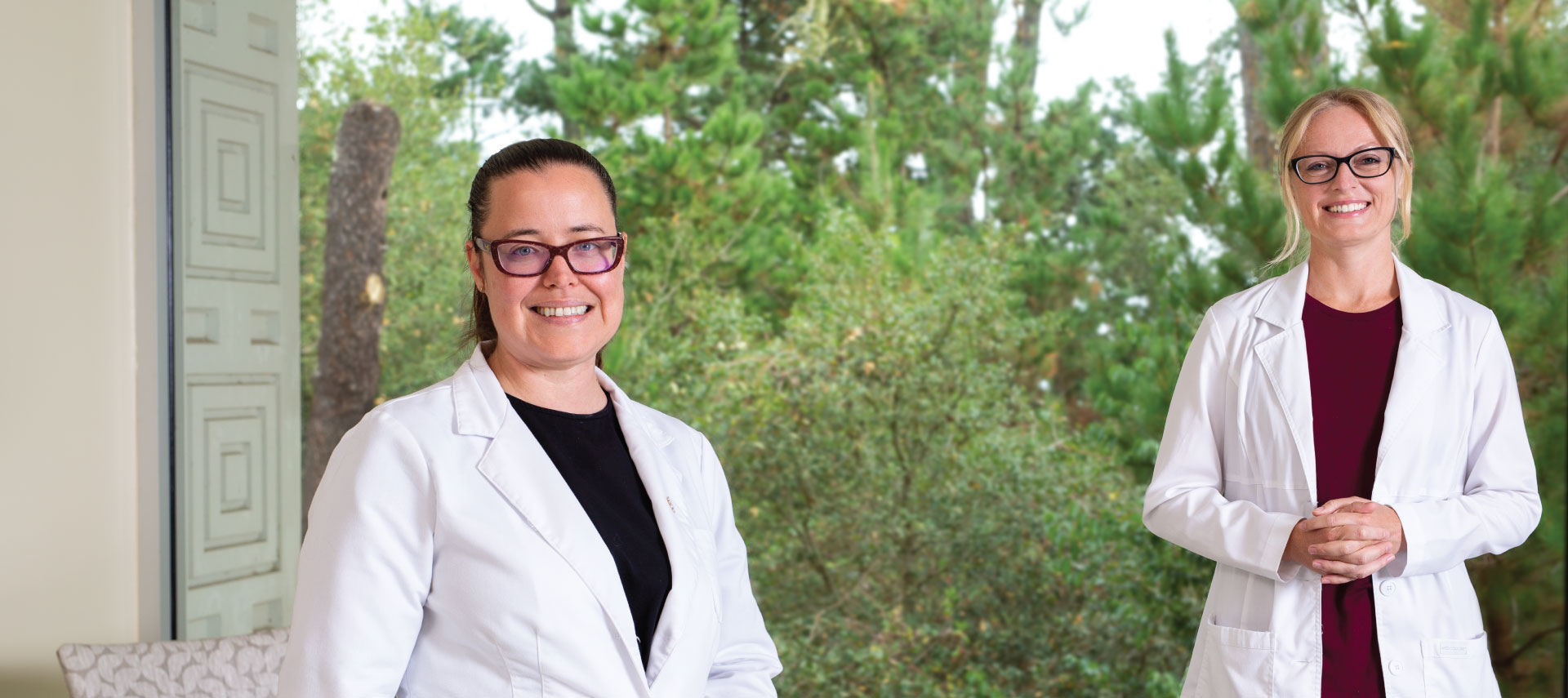
An additional human touch is provided by the nurse navigator. After meeting with a surgeon and determining that a knee, hip, or shoulder replacement is the best option, a patient connects with the Orthopedic Center at Community Hospital.
“Patients first meet with our nurse navigator, or with me, at a pre-anesthesia testing appointment,” says Sarah Wurtz-Huseby, program manager of the center. “This is the first touchpoint, where we explain our role, which is to build a bridge between the patient, the patient’s family, and the surgeon, and be that one-to-one clinical companion through the entire process.
“From that appointment on, patients always have the ability to call us, message us, or meet with us in person, through 90 days after leaving the hospital.”
In Manhard’s case, she met with nurse navigator Jessica Hare, RN, before surgery for a thorough discussion of what to expect and how best to prepare. At an appointment in the hospital’s preoperative clinic, essential tests were done and medical history gathered — a critical step for a successful surgery. After the surgery, when it was time to leave the hospital, Wurtz-Huseby had a 45-minute call with Manhard’s husband to review at-home care and monitoring for issues that might arise.
Then, as is standard practice, Hare called Manhard’s home within 48 hours of the surgery to make sure pain was under control and she had all needed medications and supplies. Follow-up calls continued every two weeks for three months, to ensure progress.
“This is the next level in comprehensive care, easing those transitions between home and hospital, then back home again after surgery,” says Hare, the designated navigator.
Also integral to the team is a “coach,” typically a family member or friend of the patient whose role is to support them at home for a minimum of three days after surgery. In Manhard’s case, it was her husband.
“We educate the coaches about the things they need to know and familiarize them with a reference guide we provide,” Meckel says. “If a patient has pain, the coach can flip to the page that addresses pain and immediately find things they can try — elevation, massage, ice, distraction, medication …”

"Joint replacement was arguably one of the most-difficult surgeries to overcome, but today is a much-easier, very-successful type of surgery."
— Dr. Michael Pitta, Orthopedic surgeon
The coach also helps the patient get in and out of bed safely, ensures that the patient attends appointments with doctors and physical therapists, and helps process information and instructions from the doctor. “It’s not unusual for a patient to forget things because of the stress of surgery,” Pitta says. “The coach is there to be the sponge that can absorb information and relay it back to the patient.”
“Joint replacement was arguably one of the most-difficult surgeries to overcome, but today is a much-easier, very-successful type of surgery,” Pitta says. He and Meckel cite numerous advances in anesthesia, pain management, post-op recovery, physical therapy, and tools and technology, including:
- The newest generation of artificial joints are composed of ultra-high molecular-weight polyethylene, more durable than previous versions, and less likely to loosen during use
- Patients previously were hospitalized 3–5 days after joint surgery, but today go home the following day in most cases. Reasons for the quicker release include improved anesthesia (spinal anesthesia, rather than gas, resulting in less nausea and fewer blood clots), more-effective pain medication (a combination to regulate pain in different ways, as opposed to a single narcotic painkiller), and elimination of a catheter (less necessary because modern surgeries are quicker)
- Joint-replacement patients once spent two weeks, and sometimes up to a month, recovering in a skilled nursing facility, but a change in philosophy has reduced the need. Bed rest no longer is encouraged, because active patients recover much more quickly. And patients also tend to do better at home, in their own, comfortable environment
“You’re not sick after joint replacement; on the day of surgery, once the anesthesia wears off, the patient needs to stand and walk,” Meckel says. “The idea that you need to stay in bed, with people bringing everything you need, is wrong. Getting out of bed to fetch your own glass of water is great therapy.”
“Community Hospital has an orthopedic floor, with orthopedic nurses who know how to care for joint patients after major surgery,” Pitta says. “We feel very fortunate that CHOMP provides us with that level of personnel, and has allowed us to bring in technology that has been shown to benefit our patients.”
Total hip replacement surgery
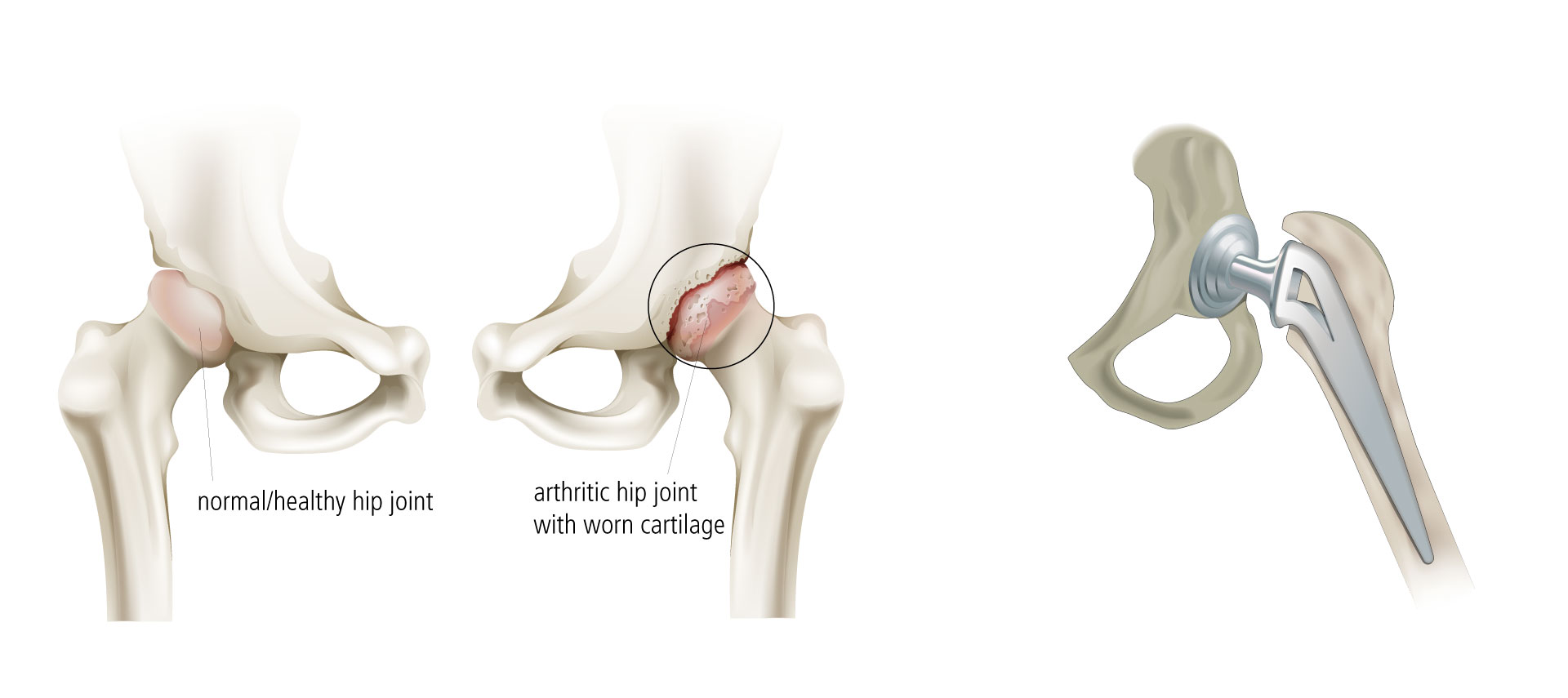
Total hip replacement surgery replaces the upper end of the thigh bone (femur) with a metal ball and resurfaces the hip socket in the pelvic bone with a metal shell and plastic liner.
Total hip replacement surgery replaces damaged cartilage with new joint material in a step-by-step process.
Doctors may attach replacement joints to the bones with or without cement.
- Cemented joints are attached to existing bone with cement
- Un-cemented joints are attached using a porous coating that adheres the bone to the artificial joint. Over time, new bone grows and fills the openings in the porous coating, attaching the joint to the bone
- There are different approaches for hip replacement surgery. If you are interested in joint replacement, discuss the various options with an orthopedic surgeon.
Total knee replacement surgery
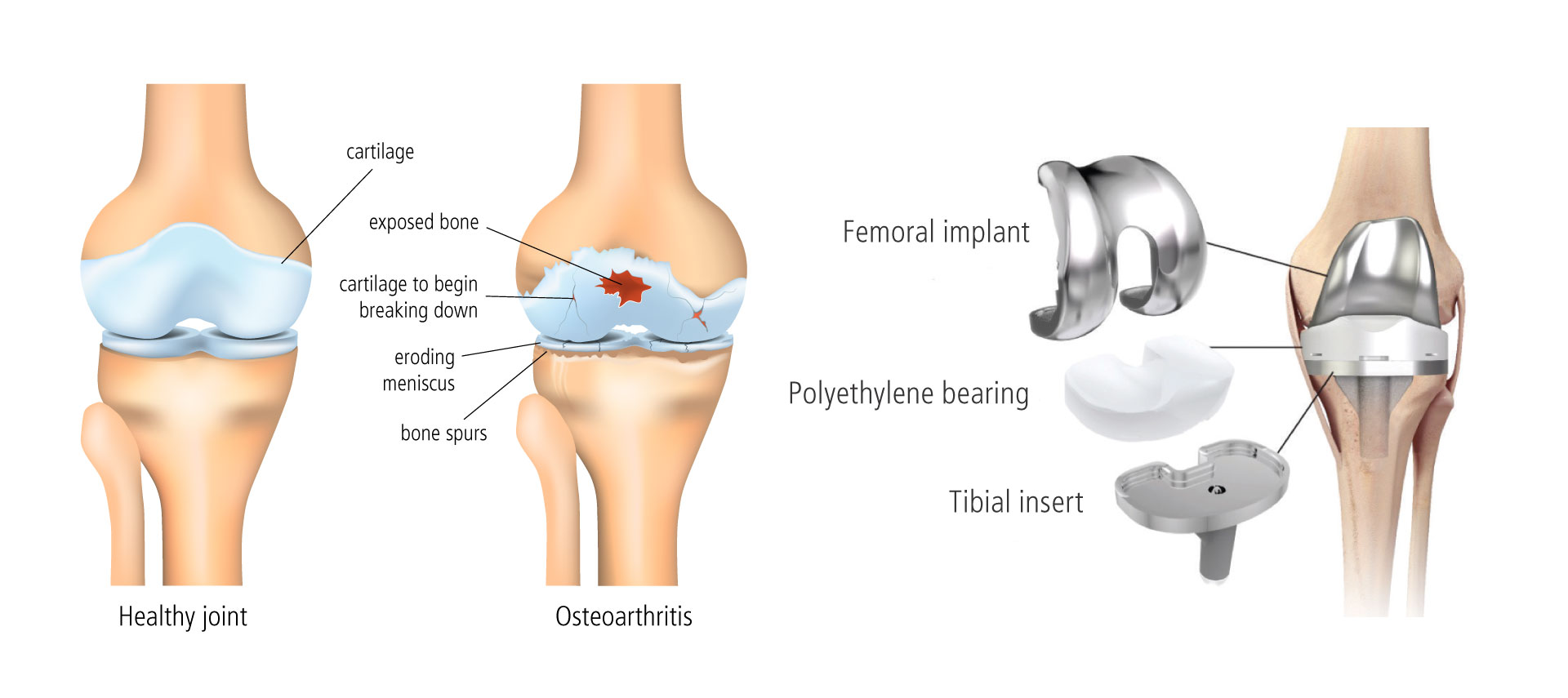
Knee replacement surgery involves replacing some or all of the components of the knee joint with a synthetic implant to repair the damaged weight-bearing surfaces that are causing pain. Total knee replacement surgery replaces all three compartments of the diseased knee joint. While there are non-surgical and surgical interventions short of knee replacement that often provide temporary relief, the long-term resolution to most knee degeneration is joint replacement.
There are two main benefits from knee replacement surgery: elimination of pain and improved range of motion. Of all possible surgical interventions, total knee replacement offers the greatest quality of life improvement and has a high success rate.