Advances in technology, medicine, and expertise combine to preserve vision in more people

A haunting memory from the ophthalmology internship of Dr. Eric Del Piero, circa 1980, is the day he perused medical records at a clinic in San Francisco and saw doctors’ notes in several files that had been written only a few years earlier: “Send patient to learn Braille,” they recommended.
“It’s humbling to remember where we were in ophthalmology 40 years ago and then compare it to where we are today,” says Del Piero, a Monterey-based retinal specialist. “It’s great to think of all the things we can do today to help patients keep their vision for their entire lifetime.”
While most eye care is provided in a doctor’s office, more serious issues are addressed in a surgical setting. In 2019, more than 800 eye procedures were performed in the Outpatient Surgery Center or the main operating room at Community Hospital of the Monterey Peninsula.
That number could grow with a remodel and enhancement of the outpatient center that will provide new tools and capabilities for preserving and protecting vision. The project, with expected completion in summer 2021, is being funded with a substantial gift to Montage Health Foundation from Carmel resident Marvin Silverman.
The project includes a dedicated procedure room and multiple advances in technology, including a transscleral laser for the treatment of glaucoma.
“We’ll also have the ability to do laser-assisted cataract surgery in the Outpatient Surgery Center, a significant upgrade that will improve the accuracy of some of the steps we now do by hand,” says Dr. Leland Rosenblum, who specializes in the treatment of cataracts and glaucoma.
The new equipment will enable procedures that could previously be performed only in Community Hospital’s main operating room.
“We’ll be able to perform more complicated surgeries than ever before on an outpatient basis,” says Del Piero, who helped design the hospital’s first ophthalmology rooms in 1990.
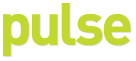
Glaucoma and cataracts are the most commonly addressed eye conditions at Community Hospital. Glaucoma is a group of eye conditions that damage the optic nerve, usually from abnormally high pressure in the eye. There is no cure, but there are treatments, including prescription eye drops, oral medications, laser treatment, surgery, or a combination.
Glaucoma
Glaucoma is a group of eye diseases that can cause vision loss and blindness by damaging the optic nerve, in the back of the eye. Primary types are:
- Open-angle glaucoma, the most common; many people don’t have symptoms until they start to lose vision.
- Angle-closure glaucoma, which develops when the outer edge of the iris (the colored part of the eye) blocks fluid from draining out of the front of the eye, causing a sudden increase in pressure. It is a medical emergency and requires treatment right away. Untreated, it can cause blindness in just a few days
Symptoms: Usually starts slowly and goes unnoticed. Over time, may lose side vision, especially closest to the nose. Angle-closure glaucoma can cause sudden symptoms including intense eye pain, upset stomach, red eye, blurry vision and requires emergency treatment
Risk factors: Anyone can get glaucoma but increased risks are for those over age 60, African American or Hispanic/Latino over age 40, family history of glaucoma
Diagnosis: Dilated eye exam
Treatment: There’s no cure, but early treatment can often stop damage and protect vision and includes medicated drops, laser treatments, and surgery
SOURCE: National Institutes of Health
“Drops are still the mainstay, but patients need more than that many times,” says Dr. Philip Penrose, an ophthalmologist in Monterey since 2005. “They may be suffering from side effects of the drops or they’re not lowering their eye pressure enough.”
To reduce fluid buildup that causes the pressure, laser therapy can be done to increase outflow through channels in the eye, or surgery can create an opening in the white of the eye to enable drainage. Doctors can also insert a tiny stent in the eye to act as a drainage tube.
“Better microscopes enable us to see in these small areas and place these stents that are about the size of the ‘1’ in the date on a penny,” Penrose says.
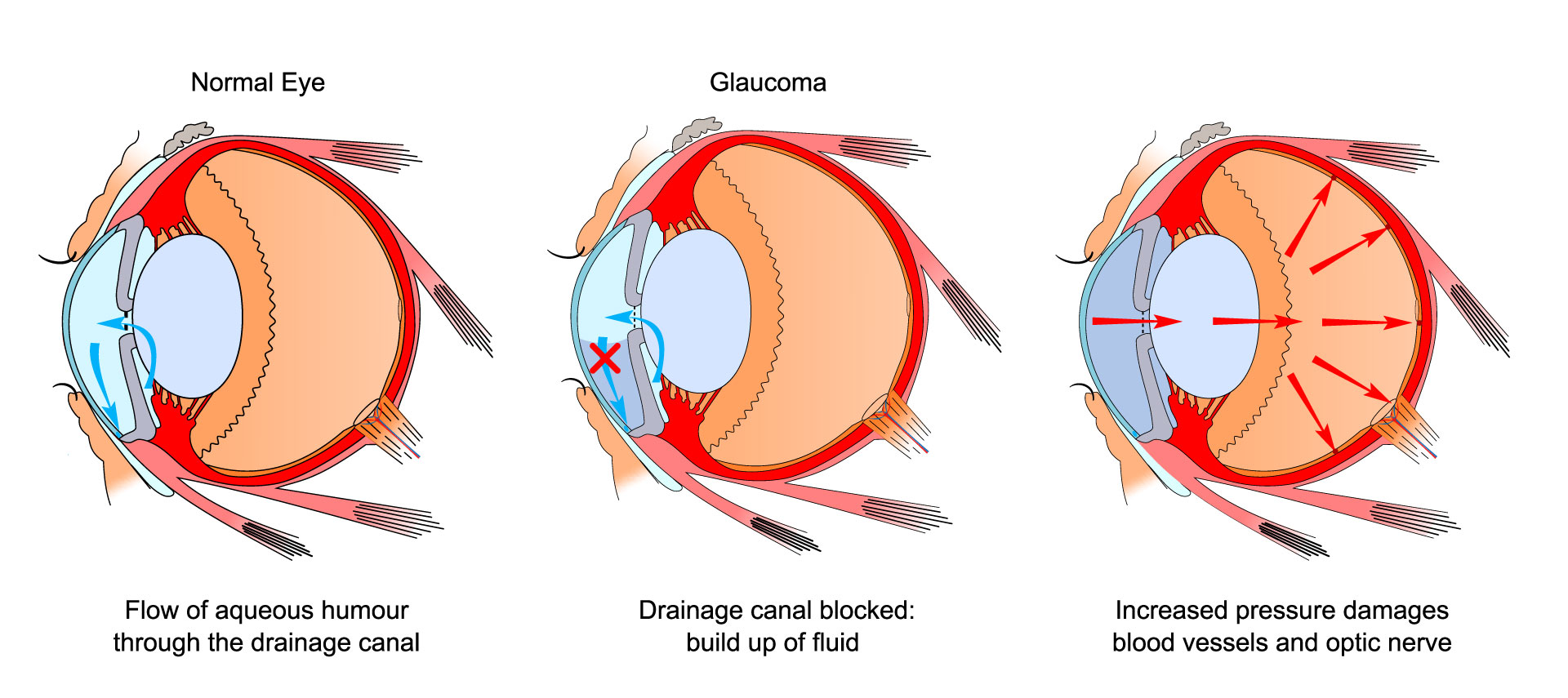
Ophthalmology was the first medical field to use microscopes in surgery, and the technology has evolved substantially in recent years. Advanced microscopes, lasers, and lenses are also improving surgery and outcomes for cataracts, when the lenses become cloudy, obscuring vision.
“The one tissue you look at and pay the most attention to in cataract surgery is the lens capsule, the thin membrane that supports the lens and keeps it centered,” says Penrose, who specializes in cataract surgery and has done more than 800 laser procedures. “You want to protect the tissue in the eye and around the cataract, especially the capsule and the cornea. You want to efficiently remove the cataract, protect the tissue, and maximize their vision so they have relatively less dependence on glasses. The technology of the microscopes we’re using is unbelievable. We can see that membrane, and micro-granules on that membrane, and make sure it’s intact during the surgery.”
Del Piero says the advances in ophthalmology during his four decades as a physician have been wondrous.
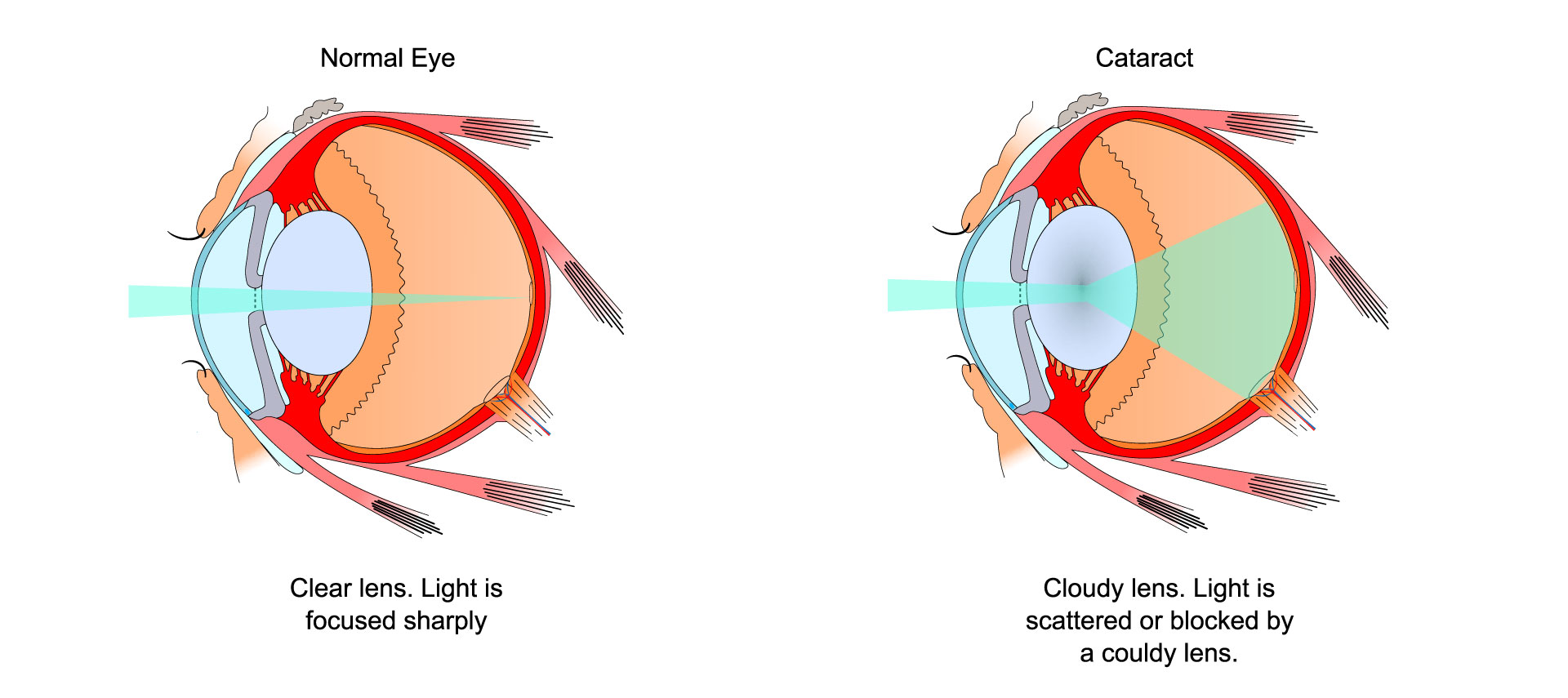
“When I did my internship in 1980 and ’81, they were using an instrument called a Xenon arc photocoagulator, which predated the lasers we use now. It was roughly the size of a small room,” he says. “It was only after we started using the Xenon arc photocoagulator and lasers that we were able to get some kind of control over the really severe diabetic retinopathy that developed in patients.
“The lasers we have today are much better; they’re very precise, and our ability to deliver them correctly is vastly improved.”
Del Piero commonly treats patients with age-related macular degeneration and retinal disease, detachments, and retinal defects.
“Those things can cause you to go blind, so we place the retina back into its normal anatomical position so it functions correctly,” he says.

Many of the surgeries Del Piero has been performing in Community Hospital’s main operating room are on patients with diabetic retinopathy and intraocular hemorrhaging. When the remodeling and enhancements are complete, he’ll be able to do those in the hospital’s Outpatient Surgery Center.
Rosenblum’s specialties include cataracts and glaucoma, including surgeries for pterygium (scar tissue that grows across the eye, caused by chronic exposure to sun and wind), YAG laser capsulotomy (scar tissue that sometimes forms behind implant lenses after cataract surgery), and trabeculoplasty and iridotomy (laser procedures to treat glaucoma).
“The technology just keeps getting better,” Rosenblum says. “We’re now able to use a laser to assist with cataract removal. We have intraocular lenses to correct for astigmatism, and multifocal lenses that correct for both nearsightedness and farsightedness.
“We have the ability now to work through very small incisions — two millimeters, or even smaller,” Rosenblum says. “We have selective lasers that don’t leave scar tissue, and selective lasers that can deliver energy across the wall of the eye to lower eye pressure in patients with glaucoma.”
The physicians also focus on prevention and nonsurgical interventions.
Glaucoma can often be treated with special eyedrops. Macular degeneration can often be thwarted by wearing effective sunglasses and a hat, and using eyedrops to reduce irritation. Many factors can contribute to cataracts, including age, family history, diabetes, smoking, too much sun exposure, and prednisone medication, says Rosenblum.
“Prevention is something I really push,” Del Piero says. “How do you prevent a diabetic from developing diabetic eye disease? By making sure primary care doctors help them keep their diabetes under control. I’m a big cheerleader for prevention.”
Cataracts
A cataract is a cloudy area in the lens of the eye. More than half of Americans 80 or older have cataracts or have had surgery to get rid of cataracts.
Symptoms: Blurry vision, faded colors, light sensitivity, trouble seeing at night, double vision
Risk factors: Risk rises with age. Other factors: certain health problems, like diabetes; smoking; too much alcohol; family history of cataracts; eye injury or surgery or radiation on upper body; a lot of time in sun; steroid use
Prevention: Quit smoking; wear sunglasses and a hat to block sun; eat more fruits and vegetables, especially dark, leafy greens
Diagnosis: Dilated eye exam
Treatment: Surgery
Diabetic retinopathy
Diabetic retinopathy affects the blood vessels in the retina (the light-sensitive layer of tissue in the back of the eye) and can cause vision loss and blindness in people who have diabetes.
Symptoms: Blurry vision, floating spots or streaks in vision, blindness
Risk factors: Any kind of diabetes
Prevention: Manage your diabetes, keeping blood sugar levels as close to normal as possible; high blood pressure and cholesterol increase the risk
Diagnosis: Dilated eye exam
Treatment: Medicine, laser treatment, surgery
SOURCE: National Institutes of Health
When should you see an ophthalmologist?
No symptoms of eye problems or risk factors:
Get a baseline eye disease screening at age 40, with follow-ups as recommended by the doctor, based on the results
With symptoms of eye problems or risk factors:
See an ophthalmologist now to determine how often to have eye exams if you have a family history of eye disease, diabetes, or high blood pressure